Modern Livestock & Poultry Production – Possible Without Antibiotics?
Introduction – Small and marginal livestock farmers are among the country’s most vulnerable citizens. Disease outbreaks in their businesses result in significant economic losses as well as resource waste. In such cases, the use of antibiotics is required. In this document, we attempt to bring out some clear hard facts that are frequently overlooked when discussing the role of food-producing animals in antibiotic resistance.
Antibiotic resistance simply means ‘antibiotics become useless’. There are many myths associated with the term antibiotic resistance. This article is aimed to burst those myths and at the same time, we will also try to see the real threat looming around.
Studies says that if AMR (Antimicrobial Resistance) is not tackled now than by 2050, 1 person could die every 3 seconds due to it. Antibiotic resistance is one of the biggest threats to global health, food security, and development today.
WHO says that antibiotic resistance is one of the biggest threats to global health, food security, and development today.
Intensive farming systems and global use of genetically evolved breeds forced us to use higher amounts of antibiotics. We cannot undermine the dependency of our livestock and poultry production system on antibiotics. Without antibiotics, these systems could simply fail to produce food.
The basic reason for dependency on antibiotics is that productivity and immunity are 2 different traits which are negatively correlated.
The genetic correlation between clinical mastitis and milk yield traits was positive (from 0.38 to 0.56), confirming the genetic antagonism between production and udder health traits. Reason could be simple that according to the concept of nutrition partitioning energy and protein is diverted towards milk production rather than immune system.

Cows are challenged by a transient decrease in feed intake resulting in negative energy and protein balance in early lactation, and short duration but substantial hypocalcemia around calving. Concurrently, there is impairment of innate immune function and regulation of inflammation which is central to the development of mastitis and uterine diseases. Highest incidence of mastitis occurs around the time of calving, and this is particularly true for coliform infections.
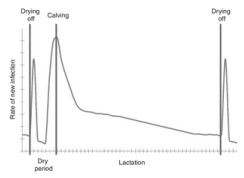
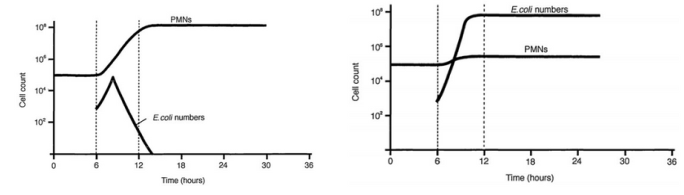
In cattle, the circulating half-life was estimated to be 9 h. Neutrophils in dairy cows in the transition period may have a shorter-than-normal lifespan. The two best-studied elements of neutrophil function in dairy cows are phagocytosis and oxidative burst. Each of retained placenta, metritis, purulent vaginal discharge, endometritis and mastitis (which collectively affect at least 25% of dairy cows in early lactation) is strongly associated with impairments of one or more aspects of neutrophil function. There are two peaks in the risk of new infection in the lactating cycle, one during involution and another centred around the time of calving. Good neutrophil response in a mid lactation cow can lead to rapid elimination of E. coli.
Modern high producing cows have inherently lower immunity and these cows around calving have further dip in immunity due to various reasons & one of them is reduced neutrophils activity. Therefore use of ANTIBIOTICS in cows become very common and further there are chances of misuse due to misdiagnosis during lower milk production.
Weak Immune system of modern poultry
Indeed, over the last 60 years, the commercial poultry breeding industry has achieved remarkable genetic progress for economic criteria such as growth rate, meat or egg production, and feed efficiency. For example, if we compared to a broiler line from the 1950s, modern broilers have a growth rate that is more than 400% faster, with a concomitant 50% reduction in feed conversion ratio (estimated as the ratio between the mass of feed consumed and the total weight gain for a particular period).
Field observations suggest that commercial chickens generally display weaker immune capacities, as indicated by an increased susceptibility to infectious diseases and reduced adaptive immune responsiveness. Resource allocation theory, from this theory (given by Beilhartz) we can expect that when an animal is genetically driven towards high production and efficiency, fewer resources will be left for other life-history traits, including immunity.
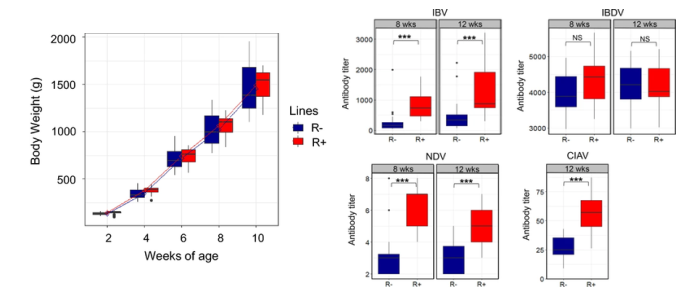
The R+ and R− chicken lines are the product of a divergent selection experiment that started in 1976, from a Rhode Island Red population of six sires and 50 dams. Chickens with a low RFI value (R−) are more efficient producers because they require less feed to reach a given body weight (BW) and level of egg production than chickens with a high RFI value (R+). Antibody titers of R+ and R− chickens, measured by ELISA or IHA (NDV) after vaccination, at 8 and 12 weeks of age. Asterisks indicate significant differences between lines.
Through experiments that have evaluated the effects of antibiotics on growth or compared chicken growth in a sterile environment compared to a conventional, pathogen-free environment, the maintenance costs of immunity have been indirectly estimated to be in the range of 5% of daily nutrient needs. Many infections, including those related to vaccination, trigger an acute phase response, which is characterized by increased protein synthesis and can account for about 9% of the body’s total nutrient use.
Commercially raised chickens also have diminished polymorphism at loci of the major histocompatibility complex that are known to be associated with disease resistance or susceptibility. Commercially raised chickens also have diminished polymorphism at loci of the major histocompatibility complex that are known to be associated with disease resistance or susceptibility.
Use of antibiotics is inevitable in food animals if production practices are compromised
With above given facts and studies conducted on various species it has been shown that immunity of modern food producing animals and birds is trade off with productivity traits and they become more prone to infections that are not harmful to these animals in general.
Further, due to high feed prices & demand, quality of feed with respect to minerals and vitamins is compromised. Mycotoxins present in feed further deteriorate immunocompetency of livestock and poultry.
Principles of prevention and biosecurity are undermined and little awareness about these 2 things are present among farmers.
Immunosuppressive viral diseases like Gumboro, IBH, Mereks & CIA causes diseases which attacks weaken immune system. CRD, E.coli and opportunistic bacterial diseases become common in farms which are tough to handle.
Vaccine reactions and vaccine induced immunosuppression also responsible for various diseases which reduces growth and even cause mortality
Antibiotics used in livestock in India
- Neomycin
- Ampicillin
- Enrofloxacin
- Marbofloxacin
- Ceftizoxime
- Azithromycin + Neomycin
- Amoxycillin + Cloxacillin
- Amoxycillin + Salbactum
- Ceftiofur (with or without tazobactum)
- Ceftriaxone (with or without tazobactum)
- Cefquinome
- Clindamycin
- Ciprofloxacin + Tinidazole
- Levofloxacin + Ornidazole
- Gentamycin
- Colistin Sulphate + Cloxacillin
- Cefoperazone
- Sulphadiazine + Trimethoprim
- Streptomycin + Penicillin
- Sulphamethoxazole + Trimethoprim
- Oxytetracycline
- Sulphadimidine
- Doxycycline
- Mupirocin
- Cephalexin
Defined Daily Dose (DDD): The assumed average maintenance dose per day for a drug used for its main indication in humans and corresponding system is also defined in animals. Tackling the problem of rising antibiotic resistance requires valid and comparable data on the use of antimicrobial drugs in livestock. To date, no harmonized monitoring of antimicrobial usage in animals is available, and there is no system to assess usage data throughout Europe, thus hampering a direct comparison between different European countries. Most of the currently applied monitoring systems are based on sales data. Placement of sales data in relation to the population at risk requires overall assumptions about the weights of the animals treated and the doses applied.
India uses 3% of global antibiotics used in food animals
At the national level, total private-sector antibiotic consumption increased by 12.0% between 2011 and 2016, from 4749 to 5358 million DDDs, and then decreased to 5071 million in 2019. Attempts to respond to the rising food demand, driven by high population growth, urbanization, and rising income, have put pressure on farmers to produce more but in limited spaces.
The global consumption of antimicrobials in food animals was estimated at 63,151 tons (±1650) tons in 2010 and at 131,109 tons in 2013. The use of antimicrobial in intensive production systems is high and explains about 34% of the global increase in consumption. A global rise of up to 200,235 tons by 2030 has been projected. India accounts for about 3% (2010) of the global consumption of antimicrobials in food animals.
The biomass of animals raised for food now exceeds the global biomass of humans. In Asia, daily animal protein intake grew from 7 grams per capita per day to 25 grams between 1960 and 2013. The proportion of the diet coming from rice and wheat progressively decreased, primarily among higher-income adults. We have earlier seen how food animals are prone to diseases due to various reasons.
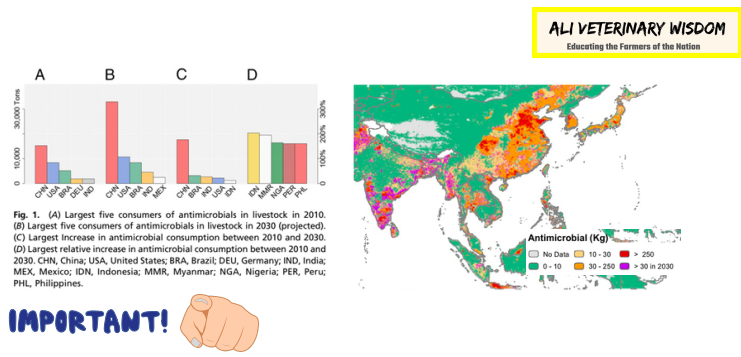
- Antibiotic consumption in poultry by 2030 would be increased by 129% in India. Currently it is around 4000 tons (3% of global).
- Total acreage of areas where antibiotic consumption is currently greater than 30 kgkm2 will increase by 143%.
- Growth in poultry industry forces high consumption areas (30 kgkm2) to increase its consumption by 312% 2030.
- China was the largest antimicrobial consumer for livestock in 2010, and by 2030, its livestock industry will consume up to 30% of global antimicrobial production.
- If current trends continue, India will contribute a significant portion of the overall increase in antimicrobial consumption in food animals—a country already dealing with antibiotic overuse in human medicine and an extremely high (and increasing) prevalence of ARBs (e.g., 95% of adults in India carry bacteria resistant to -lactam antimicrobials). Widespread resistance may be more significant for India than for other countries because India has one of the highest bacterial disease burdens in the world, and thus antimicrobials play a critical role in limiting morbidity and mortality.
- We already seen various factors which increases antibiotic consumption in animals.
Therapeutic antibiotics
- Amikacin
- Amoxycillin
- Cloxacillin
- Doxycycline
- Azithromycin
- Ampicillin
- Apramycin
- Ceftiofur
- Cephalexin
- Chloramphenicol
- Chlortetracycline
- Ciprofloxacin
- Colistin
- Neomycin
- Enrofloxacin
- Erythromycin
- Flumequine
- Furaltadone
- Furazolidone
- Gentamicin
- Levofloxacin
- Lincomycin
- Oxytetracycline
- Pefloxacin
- Tetracycline
Antibiotic growth promoters
- BMD (Bacitracin)
- Auromycin
- Erythromycin
- Chlorohydroxyquinoline
- Doxycycline
- Cephalexin
- Ciprofloxacin
- Chlortetracycline
- Colistin !
- Tiamulin
- Furazolidone
- Lincomycin
- Neomycin
- Enrofloxacin
- Pefloxacin
- Oxytetracycline
- Virginiamycin
- Enramycin
- Avilamycin
- Tylosin
How we can reduce the use of antibiotics
- Prevention of diseases through biosecurity
- Use of water sanitizer in case of poultry
- Proper cleaning programs in farms especially poultry farms
- Acidifiers in feed which slows the growth of pathogenic microbes
- Probiotics inhibit the pathogenic bacteria through competitive exclusion
- Prebiotics (lectin receptor binders) which agglutinate / neutralize pathogens
- Herbal antimicrobials and phytogenic components
- Chemical inhibitors like sodium chlorate
- Good management practices
- Use high quality toxin free feed
- Chicks should be sourced from good hatchery which follows clean hygienic practices.
- Knowledge of epidemiology of infections (especially in mastitis and metritis in cows). These things can be easily prevented.
- Use antibiotic only when it is warranted and at proper dose (As prescribed by veterinarian).
- Remember if resistance is created in farm it could transfer to you also.